What to know about cancer screenings
What to know about cancer screeningsCancer death rates are down, meaning four million fewer people have been lost thanks to better treatment and early detection—a huge win!
But cancer diagnoses are still on the rise. A bleak fact is that, this year, the U.S. is projected to cross the two million-mark for new cancer cases, according to the American Cancer Society (ACS).
What’s also alarming when it comes to trends in cancer is that many new instances of cancer are happening in younger populations.
Colorectal cancer cases are increasing in individuals younger than 55, while incidences of cervical cancer are growing in women between the ages of 30 and 44—both of which can be detected and prevented from becoming life-threatening prognoses through cancer screenings.
With cancer remaining a prevalent, if not growing, issue, costs associated with cancer diagnoses and treatment are also increasing. In 2020, researchers estimated that national costs for cancer-related medical services and drugs would grow 34% from 2015 to 2030, reaching a staggering $246 billion—up from $183 billion just nine years ago. In a recent survey of large self-funded employers, 85% of benefits managers reported oncology as a top-three cost driver, with almost half listing it as number one. These same employers expect their cancer spend to increase by an average of 9% annually for the next few years.
One of the best ways to mitigate costs and keep mortality rates low is to prioritize and emphasize the importance of cancer screenings. Guidance on how these cancer screenings work can be confusing, especially as they differ depending on the type of cancer. Here, we provide a breakdown of the most up-to-date information on cancer screenings in the U.S.
Cancer screening guidelines
In short, a cancer screening is any sort of test that looks for signs of cancer—often before a patient has shown any symptoms or experienced any concerns with their health. Screenings can come in the form of a physical exam, blood or urine test, imaging, or a genetic test, among other types of tests.
Cancer screenings aren’t foolproof, meaning there’s a risk of receiving a false positive or negative. There’s also never a guarantee that early detection will prevent cancer from spreading or becoming fatal. Nevertheless, the benefits of evidence-based cancer screenings far outweigh the risk of a false positive, and catching cancer early is always better.
Many cancer screenings take place for patients in their 40s, when they’re more at risk, but can start earlier for patients with pre-cancerous conditions and/or a family history of certain cancers.
How are cancer screening guidelines determined?
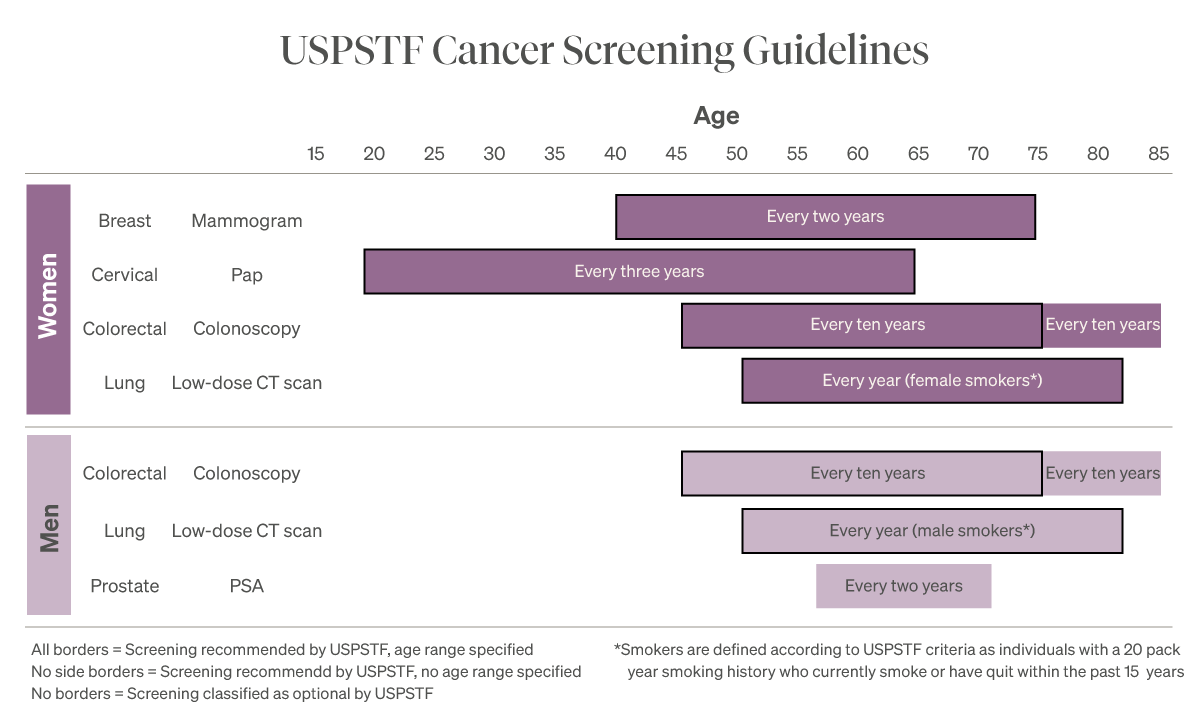
Coverage for cancer screening guidelines in this country is governed and determined by the U.S. Preventive Services Task Force (USPSTF), an independent panel of experts in disease prevention and evidence-based medicine that’s been around since the 1980s. Because medicine and science are ever-changing, so too are the USPSTF’s guidelines being updated and revised as new needs and discoveries emerge.
To add to the confusion, other major organizations such as the American Cancer Society (ACS) and the American College of Obstetrics (and more!) have their own cancer screening guidelines. Fortunately, these guidelines are usually aligned—for the most part—but there are often differences in when and how often people should be screened. As one can imagine, this can make it confusing for patients and their physicians.
For example, the ACS has been advocating for women to receive annual mammograms starting at the age of 40 for years. And though the USPSTF did change the recommended start age to 40 recently, they are still saying it should be every two years versus the ACS recommendation of every year.
What are the current U.S. cancer screening guidelines?
Unfortunately, the U.S. doesn’t have cancer screening guidelines for every type of cancer out there. This is largely due to the fact that, for cancer types without one, there is yet to be evidence that a certain screening can accurately catch that cancer or that catching it could change the outcome.
The USPSTF has guidelines for the following cancers, and experts recommend everyone get screened for them when the appropriate time comes:
- Breast cancer
- Cervical cancer
- Colorectal cancer
- Lung cancer
- Prostate cancer
Below, we’ll explain who each screening applies to and the current protocol for each.
Breast cancer screening guidelines
Just this year, the guidelines for breast cancer screenings were changed: The USPSTF determined in 2023 that routine mammograms should begin at age 40—a response to rising cases of breast cancer in women in their 40s. Previously, the starting recommended age was 50. (The ruling has caused widespread controversy, with some experts arguing earlier screenings will do more harm than good and others saying it doesn’t go far enough to protect women’s health.)
The USPSTF recommends women aged 40 to 74 get screened via mammogram and physical breast exam biannually while they’re in reasonable health. In addition, an MRI might be recommended for patients with a family history of breast cancer or genetic risks.
Cervical cancer screening guidelines
For cervical cancer screening, a doctor will conduct a Pap smear—a swab that collects cells from a patient’s cervix. A Pap smear is recommended every three years for patients between the ages of 21 and 29 (sometimes starting as late as 25), and every three to five years for those 30 years old and up (alongside an HPV test, even if the patient received the HPV vaccine). By the time a patient has reached 65, if they have have not had a positive cervical cancer result in the past 10 years, their provider might suggest stopping screenings.
Colorectal cancer screening guidelines
An unusual and unfortunate reality is that colorectal cancer is becoming more prevalent in younger adults. The good news is that it can be caught and treated early with screenings.
Experts recommend colorectal cancer screening begin at age 45 on a regular basis (about every five to 10 years for colonoscopies, the CDC reports, or more often based on personal or family history) and continue until around 75. These screenings could include a stool test (which should be completed annually), sigmoidoscopy or colonoscopy (a thin tube is inserted into the rectum to look for polyps or signs of cancer), and/or X-ray.
Lung cancer screening guidelines
Lung cancer should be screened for yearly in patients ages 50 to 80 who smoke or used to smoke at least one pack of cigarettes a day for 20 years or more. This screening is conducted via a low-dose CT scan, which takes a detailed image of the lungs.
Prostate cancer screening guidelines
The ACS recommends men should start prostate cancer screenings—a blood test and/or rectal exam every one to three years—starting at age 50, unless they have a higher risk of developing it, in which cases they should begin at age 45.
The prostate specific-antigen blood test screening (PSA) has been an area of much debate and drama over the past couple of decades. Since 2008, PSA screening rates have been dropping due to evidence that questioned the value of routine PSA screening.
In 2018, the USPSTF said the decision to be screened for prostate cancer should be an individual one for men between the ages of 55 to 69.
Since then, however, there has been a movement showing that reduced PSA screening has led to high rates of metastatic prostate cancer with a disproportionate impact across different populations, specifically the Black community.